HEALTH TRAIN EXPRESS Mission: To promulgate health education across the internet: Follow or subscribe to Health Train Express as well as Digital Health Space for all the updates for health policy, reform, public health issues. Health Train Express is published several times a week.Subscribe and receive an email alert each time it is published. Health Train Express has been published since 2006.
Monday, February 25, 2013
EHR users unhappy, many switching | Healthcare IT News
Meaningful use is challenging many providers with the requirement of reporting and adding new information in their current EMR. M.U. Stage I has been implemented, Stage II deadline is near or passed, and Stage III which is the most intrusive will be due next year (2014)
In addition to those requirements Clinical Decision Making will be the mantra for the remainder of this decade. The development of affordable Natural Language Processing will empower medical practices to integrate this aid.
For most MDs this will assist and accelerate the process by conifrming evidence based medicine and suitable references. This may reduce medico-legal incidents. It will also empower the addition of physician extenders.
HTE recommends that potential EMR users, and/or those considering making a switch to postopone a change at this time. Most of the new requirements are not yet available in current systems. Potential upgrades should be verified from current vendors. Our experience has been that many vendors who promise upgrades do not deliver. Clinical Decision Making may be available as a separate program or as a new module for your present EMR. The most functional CDM is integrated and capable of extracting information from you current system. This reduces error and time as well as affording transparency and seamless behind the scene functionality.
Sunday, February 24, 2013
Once is Enough
My apologies for yesterday’s redundant content. I am not sure what happened..must have been when I copied and pasted from my word editor into the blog… Face is red, blog is read three times….They say you have to read something three times to learn it. So that is my excuse.
Saturday, February 23, 2013
The Future Med from Singularity Hub
The Future Med from Singularity Hub has arrived on the Health Train Express. As usual the brightest minds presented new ideas already in existence and some likely developments in the near.
Singularity University was the site for FutureMed 2013 in Silicon Valley at the NASA Ames Facility It wasn't cheap but the $ 8500 USD fee provided a turnkey experience..room..board...and the chance to hang with the 1%. I suppose most people can find a way to write it off as a deduction and have Uncle Sam subsidize your educational bent.
One can chose to hear it first, smell the crowd and wallow lavishly in the sound of bling on your neighbor's wrist or neck. Or if you are like me, the lowly physician who has seen his overhead skyrocket from 35-55% to over 80%, and has had to cease and desist from charity care in favor of supporting ObamaCare, you will attend online via a number of sources ranging from streaming video to informed bloggers and national media sources.
Most of this stuff is so advanced that a delay of one day, one week, one month, or one year is not going to amount to a significant disadvantage of not attending the 'hatching'.
FutureMed is geared around six exponentially growing areas, each taught by world class experts from the worlds of medicine, biotech and innovation. These include lectures, workshops, discussions and site visits.
1. INFORMATION – DATA DRIVEN HEALTH: Digitization of healthcare, Electronic health records, Imaging Technology, Wearable devices, Wireless monitoring to ubiquitous Apps. The ‘Big Data’ explosion… from Imaging & Diagnostics to Mobile & Internet Enabled Health… Knowledge liquidity and leveraging information to enhance diagnostics, prevention and therapy…
2. PERSONALIZED MEDICINE & ‘Omics: Low cost, point of care Genomics, Proteomics, Metabolomics, Environmental monitoring… from Systems Medicine to the rapidly emerging world of Synthetic Biology and DIY-Genomics.
3. REGENERATIVE MEDICINE: Stem cells & beyond for the repair, replacement and regeneration of tissues and organs damaged by aging, trauma or disease, from cell therapy to limb regeneration. Cellular alchemy (reprogramming skin cell to cardiomyocytes) to tissue engineering and 3-D printing of organs and tissues.
4. FUTURE INTERVENTION: From Robotic Surgery, Bionic limbs and Exoskeletons, Smart pills, and Implantable Devices, to Targeted gene therapy, and ever shrinking and more capable devices, Nanomedicine.
5. NEUROMEDICINE: Real time brain imaging, Brain computer interface (BCI), Cognitive Enhancement, Targeted neurointervention, Psychiatry and Behavioral Medicine.
6. MEDTECH/BIOTECH & ENTREPRENEURSHIP: Includes the future of Pharma and Drug Discovery, Synthetic Biology, Medical Device Development and the funding, opportunities and barriers (regulatory and otherwise) of biomedical innovation. The Drive to lower costs and more effective therapies. Impact of the FDA to Healthcare Models (Accountable Care Organizations).
The program focuses on three specific Application Areas, specifically the Future of…
MEDICAL PRACTICE & PATIENT ENGAGEMENT: How will convergent technologies impact the practice of medicine, diagnostics and clinical decision support, to new models of care from concierge practices to telemedicine… from feedback loops with patients utilizing wearable physiologic monitors, the networked ‘Medical home’ and beyond. Can care get better and at lower costs? How will better informed, engaged and socially connected patients interact with the healthcare system?
HEALTH & WELLNESS:How will personalization, nutrigenomics and regenerative medicine impact wellness, prevention and longevity?
GLOBAL HEALTH: Leveraging technology for the developing world, and learning lessons from the underdeveloped to apply in ours, from rapid viral detection & forcasting and vaccine development to strategies to prevent and treat disease in underserved and remote communities.
Here are some specifics:
FutureMed Schedule: FutureMed Singularity University: FutureMed2013: Highlights of 2013
Perhaps one of the week’s most inspiring moments came when Jack Andraka’s 15-minute talk, “The Future of Oncology,” brought the room to its feet on Tuesday. Though Andraka is but a sophomore in high school, he’s invented a new diagnostic technique for pancreatic cancer using carbon nanotubes.
Catherine Mohr, Director of Medical Research at Intuitive Surgical, delivered a fascinating lecture on the future of robotic surgery. Robotic surgery isn’t itself the disruptive technology, she said. Rather, as cutting edge diagnostic tools on the molecular level allow oncologists to diagnose earlier and earlier, surgeons will need to remove smaller and smaller tumors. Put simply, robotic surgical systems won’t drive this change—they’ll need to adapt to it.
Big data was another prime theme this year. Information that was once limited to a few select individuals in a lab or exclusive scientific community is now available to the public at large. Never mind credentials—great ideas can come from outsiders, peeking in with fresh eyes and a beginner’s mind. Indeed, Andraka used Google, Wikipedia, and free online journal articles to do the initial research behind his diagnostic invention.
Stanford’s Atul Butte told participants, “We’re drowning in data.” Butte’s Stanford lab outsources experiments, finding it more efficient to simply buy data for analysis. Just as kids in garages once built computers, incoming generations will create “garage pharma” and “dormroom biotech.”
Kohn’s session was paired with famed investor Vinod Khosla who spoke of decreasing the need for physicians and leveraging big data and data analytics to improve diagnostics and outcomes. And later in the week, FutureMed welcomed Dr. Farzad Mostashari, National Coordinator for Health and Information Technology. Mostashari said that by leveraging more connected medical records we can dramatically improve outcomes.
Andrew Hessel on synthetic biology—the use of DNA as a programming language to build living systems from the ground up.
Alan Russel on regenerative medicine and how to speed the body’s natural ability to heal itself.
The Computer History Museum capped the program with a day of demos, talks, and a pitch contest by 17 biotech and health startups from around the world. Singularity University alum, Erez Livneh, won the pitch contest with his company Vecoy Nanomedicines. Vecoy makes nanoparticle “virus traps” that mimic human cells and lure viruses (eg., HIV, influenza, hepatitis, herpes) to attack them—once lured into the trap, the nanoparticles inactivate the virus.
And now for the Star Trek 'Tricorder', once science fiction and now almost a reality.
The Future Med from Singularity Hub has arrived on the Health Train Express. As usual the brightest minds presented new ideas already in existence and some likely developments in the near.
Singularity University was the site for FutureMed 2013 in Silicon Valley at the NASA Ames Facility It wasn't cheap but the $ 8500 USD fee provided a turnkey experience..room..board...and the chance to hang with the 1%. I suppose most people can find a way to write it off as a deduction and have Uncle Sam subsidize your educational bent.
One can chose to hear it first, smell the crowd and wallow lavishly in the sound of bling on your neighbor's wrist or neck. Or if you are like me, the lowly physician who has seen his overhead skyrocket from 35-55% to over 80%, and has had to cease and desist from charity care in favor of supporting ObamaCare, you will attend online via a number of sources ranging from streaming video to informed bloggers and national media sources.
Most of this stuff is so advanced that a delay of one day, one week, one month, or one year is not going to amount to a significant disadvantage of not attending the 'hatching'.
FutureMed is geared around six exponentially growing areas, each taught by world class experts from the worlds of medicine, biotech and innovation. These include lectures, workshops, discussions and site visits.
1. INFORMATION – DATA DRIVEN HEALTH: Digitization of healthcare, Electronic health records, Imaging Technology, Wearable devices, Wireless monitoring to ubiquitous Apps. The ‘Big Data’ explosion… from Imaging & Diagnostics to Mobile & Internet Enabled Health… Knowledge liquidity and leveraging information to enhance diagnostics, prevention and therapy…
2. PERSONALIZED MEDICINE & ‘Omics: Low cost, point of care Genomics, Proteomics, Metabolomics, Environmental monitoring… from Systems Medicine to the rapidly emerging world of Synthetic Biology and DIY-Genomics.
3. REGENERATIVE MEDICINE: Stem cells & beyond for the repair, replacement and regeneration of tissues and organs damaged by aging, trauma or disease, from cell therapy to limb regeneration. Cellular alchemy (reprogramming skin cell to cardiomyocytes) to tissue engineering and 3-D printing of organs and tissues.
4. FUTURE INTERVENTION: From Robotic Surgery, Bionic limbs and Exoskeletons, Smart pills, and Implantable Devices, to Targeted gene therapy, and ever shrinking and more capable devices, Nanomedicine.
5. NEUROMEDICINE: Real time brain imaging, Brain computer interface (BCI), Cognitive Enhancement, Targeted neurointervention, Psychiatry and Behavioral Medicine.
6. MEDTECH/BIOTECH & ENTREPRENEURSHIP: Includes the future of Pharma and Drug Discovery, Synthetic Biology, Medical Device Development and the funding, opportunities and barriers (regulatory and otherwise) of biomedical innovation. The Drive to lower costs and more effective therapies. Impact of the FDA to Healthcare Models (Accountable Care Organizations).
The program focuses on three specific Application Areas, specifically the Future of…
MEDICAL PRACTICE & PATIENT ENGAGEMENT: How will convergent technologies impact the practice of medicine, diagnostics and clinical decision support, to new models of care from concierge practices to telemedicine… from feedback loops with patients utilizing wearable physiologic monitors, the networked ‘Medical home’ and beyond. Can care get better and at lower costs? How will better informed, engaged and socially connected patients interact with the healthcare system?
HEALTH & WELLNESS:How will personalization, nutrigenomics and regenerative medicine impact wellness, prevention and longevity?
GLOBAL HEALTH: Leveraging technology for the developing world, and learning lessons from the underdeveloped to apply in ours, from rapid viral detection & forcasting and vaccine development to strategies to prevent and treat disease in underserved and remote communities.
Here are some specifics:
FutureMed Schedule: FutureMed Singularity University: FutureMed2013: Highlights of 2013
Perhaps one of the week’s most inspiring moments came when Jack Andraka’s 15-minute talk, “The Future of Oncology,” brought the room to its feet on Tuesday. Though Andraka is but a sophomore in high school, he’s invented a new diagnostic technique for pancreatic cancer using carbon nanotubes.
Catherine Mohr, Director of Medical Research at Intuitive Surgical, delivered a fascinating lecture on the future of robotic surgery. Robotic surgery isn’t itself the disruptive technology, she said. Rather, as cutting edge diagnostic tools on the molecular level allow oncologists to diagnose earlier and earlier, surgeons will need to remove smaller and smaller tumors. Put simply, robotic surgical systems won’t drive this change—they’ll need to adapt to it.
Big data was another prime theme this year. Information that was once limited to a few select individuals in a lab or exclusive scientific community is now available to the public at large. Never mind credentials—great ideas can come from outsiders, peeking in with fresh eyes and a beginner’s mind. Indeed, Andraka used Google, Wikipedia, and free online journal articles to do the initial research behind his diagnostic invention.
Stanford’s Atul Butte told participants, “We’re drowning in data.” Butte’s Stanford lab outsources experiments, finding it more efficient to simply buy data for analysis. Just as kids in garages once built computers, incoming generations will create “garage pharma” and “dormroom biotech.”
Kohn’s session was paired with famed investor Vinod Khosla who spoke of decreasing the need for physicians and leveraging big data and data analytics to improve diagnostics and outcomes. And later in the week, FutureMed welcomed Dr. Farzad Mostashari, National Coordinator for Health and Information Technology. Mostashari said that by leveraging more connected medical records we can dramatically improve outcomes.
Andrew Hessel on synthetic biology—the use of DNA as a programming language to build living systems from the ground up.
Alan Russel on regenerative medicine and how to speed the body’s natural ability to heal itself.
The Computer History Museum capped the program with a day of demos, talks, and a pitch contest by 17 biotech and health startups from around the world. Singularity University alum, Erez Livneh, won the pitch contest with his company Vecoy Nanomedicines. Vecoy makes nanoparticle “virus traps” that mimic human cells and lure viruses (eg., HIV, influenza, hepatitis, herpes) to attack them—once lured into the trap, the nanoparticles inactivate the virus.
And now for the Star Trek 'Tricorder', once science fiction and now almost a reality.
The Future Med from Singularity Hub has arrived on the Health Train Express. As usual the brightest minds presented new ideas already in existence and some likely developments in the near.
Singularity University was the site for FutureMed 2013 in Silicon Valley at the NASA Ames Facility It wasn't cheap but the $ 8500 USD fee provided a turnkey experience..room..board...and the chance to hang with the 1%. I suppose most people can find a way to write it off as a deduction and have Uncle Sam subsidize your educational bent.
One can chose to hear it first, smell the crowd and wallow lavishly in the sound of bling on your neighbor's wrist or neck. Or if you are like me, the lowly physician who has seen his overhead skyrocket from 35-55% to over 80%, and has had to cease and desist from charity care in favor of supporting ObamaCare, you will attend online via a number of sources ranging from streaming video to informed bloggers and national media sources.
Most of this stuff is so advanced that a delay of one day, one week, one month, or one year is not going to amount to a significant disadvantage of not attending the 'hatching'.
FutureMed is geared around six exponentially growing areas, each taught by world class experts from the worlds of medicine, biotech and innovation. These include lectures, workshops, discussions and site visits.
1. INFORMATION – DATA DRIVEN HEALTH: Digitization of healthcare, Electronic health records, Imaging Technology, Wearable devices, Wireless monitoring to ubiquitous Apps. The ‘Big Data’ explosion… from Imaging & Diagnostics to Mobile & Internet Enabled Health… Knowledge liquidity and leveraging information to enhance diagnostics, prevention and therapy…
2. PERSONALIZED MEDICINE & ‘Omics: Low cost, point of care Genomics, Proteomics, Metabolomics, Environmental monitoring… from Systems Medicine to the rapidly emerging world of Synthetic Biology and DIY-Genomics.
3. REGENERATIVE MEDICINE: Stem cells & beyond for the repair, replacement and regeneration of tissues and organs damaged by aging, trauma or disease, from cell therapy to limb regeneration. Cellular alchemy (reprogramming skin cell to cardiomyocytes) to tissue engineering and 3-D printing of organs and tissues.
4. FUTURE INTERVENTION: From Robotic Surgery, Bionic limbs and Exoskeletons, Smart pills, and Implantable Devices, to Targeted gene therapy, and ever shrinking and more capable devices, Nanomedicine.
5. NEUROMEDICINE: Real time brain imaging, Brain computer interface (BCI), Cognitive Enhancement, Targeted neurointervention, Psychiatry and Behavioral Medicine.
6. MEDTECH/BIOTECH & ENTREPRENEURSHIP: Includes the future of Pharma and Drug Discovery, Synthetic Biology, Medical Device Development and the funding, opportunities and barriers (regulatory and otherwise) of biomedical innovation. The Drive to lower costs and more effective therapies. Impact of the FDA to Healthcare Models (Accountable Care Organizations).
The program focuses on three specific Application Areas, specifically the Future of…
MEDICAL PRACTICE & PATIENT ENGAGEMENT: How will convergent technologies impact the practice of medicine, diagnostics and clinical decision support, to new models of care from concierge practices to telemedicine… from feedback loops with patients utilizing wearable physiologic monitors, the networked ‘Medical home’ and beyond. Can care get better and at lower costs? How will better informed, engaged and socially connected patients interact with the healthcare system?
HEALTH & WELLNESS:How will personalization, nutrigenomics and regenerative medicine impact wellness, prevention and longevity?
GLOBAL HEALTH: Leveraging technology for the developing world, and learning lessons from the underdeveloped to apply in ours, from rapid viral detection & forcasting and vaccine development to strategies to prevent and treat disease in underserved and remote communities.
Here are some specifics:
FutureMed Schedule: FutureMed Singularity University: FutureMed2013: Highlights of 2013
Perhaps one of the week’s most inspiring moments came when Jack Andraka’s 15-minute talk, “The Future of Oncology,” brought the room to its feet on Tuesday. Though Andraka is but a sophomore in high school, he’s invented a new diagnostic technique for pancreatic cancer using carbon nanotubes.
Catherine Mohr, Director of Medical Research at Intuitive Surgical, delivered a fascinating lecture on the future of robotic surgery. Robotic surgery isn’t itself the disruptive technology, she said. Rather, as cutting edge diagnostic tools on the molecular level allow oncologists to diagnose earlier and earlier, surgeons will need to remove smaller and smaller tumors. Put simply, robotic surgical systems won’t drive this change—they’ll need to adapt to it.
Big data was another prime theme this year. Information that was once limited to a few select individuals in a lab or exclusive scientific community is now available to the public at large. Never mind credentials—great ideas can come from outsiders, peeking in with fresh eyes and a beginner’s mind. Indeed, Andraka used Google, Wikipedia, and free online journal articles to do the initial research behind his diagnostic invention.
Stanford’s Atul Butte told participants, “We’re drowning in data.” Butte’s Stanford lab outsources experiments, finding it more efficient to simply buy data for analysis. Just as kids in garages once built computers, incoming generations will create “garage pharma” and “dormroom biotech.”
Kohn’s session was paired with famed investor Vinod Khosla who spoke of decreasing the need for physicians and leveraging big data and data analytics to improve diagnostics and outcomes. And later in the week, FutureMed welcomed Dr. Farzad Mostashari, National Coordinator for Health and Information Technology. Mostashari said that by leveraging more connected medical records we can dramatically improve outcomes.
Andrew Hessel on synthetic biology—the use of DNA as a programming language to build living systems from the ground up.
Alan Russel on regenerative medicine and how to speed the body’s natural ability to heal itself.
The Computer History Museum capped the program with a day of demos, talks, and a pitch contest by 17 biotech and health startups from around the world. Singularity University alum, Erez Livneh, won the pitch contest with his company Vecoy Nanomedicines. Vecoy makes nanoparticle “virus traps” that mimic human cells and lure viruses (eg., HIV, influenza, hepatitis, herpes) to attack them—once lured into the trap, the nanoparticles inactivate the virus.
The Future Med from Singularity Hub has arrived on the Health Train Express. As usual the brightest minds presented new ideas already in existence and some likely developments in the near.
Singularity University was the site for FutureMed 2013 in Silicon Valley at the NASA Ames Facility It wasn't cheap but the $ 8500 USD fee provided a turnkey experience..room..board...and the chance to hang with the 1%. I suppose most people can find a way to write it off as a deduction and have Uncle Sam subsidize your educational bent.
One can chose to hear it first, smell the crowd and wallow lavishly in the sound of bling on your neighbor's wrist or neck. Or if you are like me, the lowly physician who has seen his overhead skyrocket from 35-55% to over 80%, and has had to cease and desist from charity care in favor of supporting ObamaCare, you will attend online via a number of sources ranging from streaming video to informed bloggers and national media sources.
Most of this stuff is so advanced that a delay of one day, one week, one month, or one year is not going to amount to a significant disadvantage of not attending the 'hatching'.
FutureMed is geared around six exponentially growing areas, each taught by world class experts from the worlds of medicine, biotech and innovation. These include lectures, workshops, discussions and site visits.
1. INFORMATION – DATA DRIVEN HEALTH: Digitization of healthcare, Electronic health records, Imaging Technology, Wearable devices, Wireless monitoring to ubiquitous Apps. The ‘Big Data’ explosion… from Imaging & Diagnostics to Mobile & Internet Enabled Health… Knowledge liquidity and leveraging information to enhance diagnostics, prevention and therapy…
2. PERSONALIZED MEDICINE & ‘Omics: Low cost, point of care Genomics, Proteomics, Metabolomics, Environmental monitoring… from Systems Medicine to the rapidly emerging world of Synthetic Biology and DIY-Genomics.
3. REGENERATIVE MEDICINE: Stem cells & beyond for the repair, replacement and regeneration of tissues and organs damaged by aging, trauma or disease, from cell therapy to limb regeneration. Cellular alchemy (reprogramming skin cell to cardiomyocytes) to tissue engineering and 3-D printing of organs and tissues.
4. FUTURE INTERVENTION: From Robotic Surgery, Bionic limbs and Exoskeletons, Smart pills, and Implantable Devices, to Targeted gene therapy, and ever shrinking and more capable devices, Nanomedicine.
5. NEUROMEDICINE: Real time brain imaging, Brain computer interface (BCI), Cognitive Enhancement, Targeted neurointervention, Psychiatry and Behavioral Medicine.
6. MEDTECH/BIOTECH & ENTREPRENEURSHIP: Includes the future of Pharma and Drug Discovery, Synthetic Biology, Medical Device Development and the funding, opportunities and barriers (regulatory and otherwise) of biomedical innovation. The Drive to lower costs and more effective therapies. Impact of the FDA to Healthcare Models (Accountable Care Organizations).
The program focuses on three specific Application Areas, specifically the Future of…
MEDICAL PRACTICE & PATIENT ENGAGEMENT: How will convergent technologies impact the practice of medicine, diagnostics and clinical decision support, to new models of care from concierge practices to telemedicine… from feedback loops with patients utilizing wearable physiologic monitors, the networked ‘Medical home’ and beyond. Can care get better and at lower costs? How will better informed, engaged and socially connected patients interact with the healthcare system?
HEALTH & WELLNESS:How will personalization, nutrigenomics and regenerative medicine impact wellness, prevention and longevity?
GLOBAL HEALTH: Leveraging technology for the developing world, and learning lessons from the underdeveloped to apply in ours, from rapid viral detection & forcasting and vaccine development to strategies to prevent and treat disease in underserved and remote communities.
Here are some specifics:
FutureMed Schedule: FutureMed Singularity University: FutureMed2013: Highlights of 2013
Perhaps one of the week’s most inspiring moments came when Jack Andraka’s 15-minute talk, “The Future of Oncology,” brought the room to its feet on Tuesday. Though Andraka is but a sophomore in high school, he’s invented a new diagnostic technique for pancreatic cancer using carbon nanotubes.
Catherine Mohr, Director of Medical Research at Intuitive Surgical, delivered a fascinating lecture on the future of robotic surgery. Robotic surgery isn’t itself the disruptive technology, she said. Rather, as cutting edge diagnostic tools on the molecular level allow oncologists to diagnose earlier and earlier, surgeons will need to remove smaller and smaller tumors. Put simply, robotic surgical systems won’t drive this change—they’ll need to adapt to it.
Big data was another prime theme this year. Information that was once limited to a few select individuals in a lab or exclusive scientific community is now available to the public at large. Never mind credentials—great ideas can come from outsiders, peeking in with fresh eyes and a beginner’s mind. Indeed, Andraka used Google, Wikipedia, and free online journal articles to do the initial research behind his diagnostic invention.
Stanford’s Atul Butte told participants, “We’re drowning in data.” Butte’s Stanford lab outsources experiments, finding it more efficient to simply buy data for analysis. Just as kids in garages once built computers, incoming generations will create “garage pharma” and “dormroom biotech.”
Kohn’s session was paired with famed investor Vinod Khosla who spoke of decreasing the need for physicians and leveraging big data and data analytics to improve diagnostics and outcomes. And later in the week, FutureMed welcomed Dr. Farzad Mostashari, National Coordinator for Health and Information Technology. Mostashari said that by leveraging more connected medical records we can dramatically improve outcomes.
Andrew Hessel on synthetic biology—the use of DNA as a programming language to build living systems from the ground up.
Alan Russel on regenerative medicine and how to speed the body’s natural ability to heal itself.
The Computer History Museum capped the program with a day of demos, talks, and a pitch contest by 17 biotech and health startups from around the world. Singularity University alum, Erez Livneh, won the pitch contest with his company Vecoy Nanomedicines. Vecoy makes nanoparticle “virus traps” that mimic human cells and lure viruses (eg., HIV, influenza, hepatitis, herpes) to attack them—once lured into the trap, the nanoparticles inactivate the virus.
And now for the Star Trek 'Tricorder', once science fiction and now almost a reality.
Friday, February 22, 2013
Obama Care Shock (and) Awe
ObamaCare Shockers
I have always stated that Obamacare would have unintended consequences and negative effects that require some level of interest in how insurance really works when coupled with an eligibility system derived from the welfare system.
In what Paul Craig Roberts calls the most comprehensive analysis available on ObamaCare, a person who wishes to remain anonymous explains how Obama Care “works for the insurance companies but not for you”
Obamacare, a Deception
Lower-income Americans who receive a subsidy to buy mandated insurance may have to pay it back if their income increases. In other words, instead of an expected tax refund they will get a bill. Note that the subsidy (“advance tax credit”) was paid to the insurance company, but the payback comes from the individual.
Persons eligible for Medicaid cannot receive a tax credit. If an Exchange finds a person to be eligible for Medicaid, he will be enrolled. Some states will auto-enroll people in Medicaid who appear to be eligible when they apply for another program such as SNAP (food stamps). If their income changes, people may be bounced back and forth from Medicaid to a tax-subsidized plan.
If a person is put into Medicaid, he has just gotten a mandated collateral loan if he uses Medicaid benefits at age 55 or older. Depending on state law, anything in the estate (the multi-generational family home and everything in it, annuities, bank accounts, etc.) may be subject to state recovery of funds expended by Medicaid for certain benefits, or possibly of all expenditures. This happens because the asset test was dropped as part of the Omnibus Budget Reconciliation Act of 1993 (OBRA 1993). While this provision does not come from the Affordable Care Act (ACA), ObamaCare’s Medicaid expansion means it can be applied much more widely. “Recovery provides revenue for cash-strapped states and it’s a big business,” the article states. It is not clear how disclosure of this provision will be made if people are bumped into Medicaid or auto-enrolled.
For some reason, getting people to enroll in ObamaCare is expected to require a high-pressure sales pitch. Enter “Enroll America,” a tax-exempt organization backed by Big Insurance. Spin experts are working on what to say and what not to say.
So, let's say you are currently unemployed, or underemployed and you do qualify for one of these Health Benefit Exchange subsidized plans and you sign up for the year. Six months into the year you are hired ! Surprise you now have to pay back whatever the subsidy amounted to. As Paul Craig Roberts writes in the Institute for Political Economy, It's very complicated”.
Come April 15th of each year you will now need a CPA, a tax specialist, a health insurance expert, and another volume of the IRS Tax Code.
Thursday, February 21, 2013
Social Media Events
It’s a great day for social ! Outdoors, indoors, or on the internet. Here’s why I jog in the morning. The view is of Mount Wilson in the distance…
Monday, February 18, 2013
Zeitgeist and Health Train Express
How many of my fellow Google Plussers know what Zeitgeist is all about? I admit I did not know until a few hours ago when I was preparing a story about the future of healthcare and medicine. What I realized immediately is that the future of healthcare and medical advances has nothing to do with medicine or healthcare, by themselves.
I spent the greater part of today, a Saturday to think about Ben Carson MD and his presentation at the National Prayer Breakfast. I spoke about the presentation in an earlier blog post.
It set off a chain of topics connected by my stumbling upon a series of TEDMED events and Singularity University. It connects great minds and great expectations via Futuremed 2013.
Finally for today and the rest of February 18-22nd 2013 Social Media Week #smw13 is taking place around the globe, with events in New York, Washington, D.C. Milan, Paris, Laga,Singapore, Copenhagen,Bogota, Chicago,Hong Kong, London, Los Angeles, Sao Paolo, Seoul, Shangai, Torina, and Vancouver.
It seems appropriate discussing Google Zeitgeist since plus has become another thread in the fabric of social media. 2012 was an awesome year, and 2013 promises to be even better
Health Train Express will focus on health related topics in social media around the globe.
The week will bring together the world of social media…different views from different cultures. Social media will bring it together….social media is a form of information exchange.
Recharge, renew, innovate, greet change with enthusiasm, lead, or be lead.
Saturday, February 16, 2013
Ben Carson M.D. Keynotes National Prayer Breakfast
Ben Carson M.D. (podium) advising Barak Obama at the National Prayer Breakfast (February, 2013)
It’s not often that a physician gets 2 million YouTube video hits in 24 hours.
One of my favorite role models has always been a pediatric neurosurgeon from the Johns Hopkins University. As a pediatrician he touches the lives of many young people, mentors young doctors and developed the procedure for separating twins joined at the skull
Ben Carson’s appearance and speech should bring no surprise to anyone who chose him for the role at the National Prayer Breakfast as the keynote speaker earlier this week. As he stood immediately to the President's position, some in the audience had a measure of discomfort.
Carson's background should be no surprise to anyone, since he has written or coauthored several books on his subject.
The power of his words on a major national platform, first the prayer breakfast and then FOXnews should give open-minded economists, politicians, and patients food for thought.
Not only does he talk the talk, he walks the walk. His speech was the real picture of the “State of the Nation”, not the idealogy of President Barak Obama, nor the opposition. Audience reaction in real time indicated the overwhelming agreement of both Republicans, Democrats, and Independents, alike.
Juan Williams and Keith Ablow MD who both are FOXnew consultants wrote about the content of Carson's speech.
Ablow compares Carson's role as a neurosurgeon,
“ Well, let me tell you something about Ben Carson and other surgeons I was privileged to train with at Johns Hopkins during my medical and surgical rotations before I chose to become a psychiatrist: They don’t pull punches when a battle needs to be joined, and they don’t hate the people to whom they have to deliver bad news.
Ben Carson has sat with many, many families and told them that their children had tumors growing inside their heads and that he would need to cut open their skulls and remove those malignancies.
Why? Because, for him, the truth is the only thing worth speaking, no matter the audience. Another thing about Ben Carson and other surgeons I scrubbed in with: They like to leave clean margins. That means that when they see pathology—like cancer—they want to cut it away so that only healthy tissue is left behind. They have to be willing to make people bleed, in order to make them live.
“ Ben Carson is my hero !” Conservative, mostly white Republican critics of the president are praising Dr. Carson because they are ecstatic to see a black man express conservative ideas to the face of a liberal, Democrat and black president’s face. But that is not why I consider Dr. Carson a hero.
He is a winner to me for living by the conservative principles I want young America, especially poor black and Latino kids, to see as the prescription for success.”
Williams goes on to elaborate,
“This was the central theme of my 2006 book, “Enough”
“PC (Political Correctness) is dangerous. In this country, one of the founding principles was freedom of thought and freedom of expression...” Carson said.
“We have imposed upon people restrictions on what they can say, on what they can think. And the media is the largest proponent of this, crucifying people who say things really quite innocently.
Williams follows up,
“As the author of a 2011 book titled “Muzzled: the Assault on Honest Debate” about how PC is dangerous and imposes restrictions on what people can say and think, this warmed my heart.
 Keith AblowM.D. is a psychiatrist who is a consultant to FOXnews.
Keith AblowM.D. is a psychiatrist who is a consultant to FOXnews.
And finally Keith Ablow comments on Dr Carson's approach to health care, coupling a flat tax, health savings accounts, minimizing the role of government and insurance companies to catastrophic insurance coverage.
Juan Williams concludes,
“The Wall Street Journal recently published an editorial headlined: “Ben Carson for President.” It said: “The Johns Hopkins neurosurgeon may not be politically correct, but he's closer to correct than we've heard in years.”
That’s true. But let’s not get ahead of ourselves with talk of a Carson presidential bid. For now, I’m just happy to see Dr. Carson celebrated as an example of the personal success that is possible in America for anyone willing to follow the basic steps of personal responsibility for their own future.
Ben Carson's ideas are not much different than mine. I cannot speak for physicians' thoughts on the state of America, today.
Friday, February 8, 2013
Health Care Reform and Political Correctness is an Oxymoron
During the past two years we have seen political demagoguery at it’s finest, and it has served neither side of the argument well. We see it in the financial world, and now it is present in health care. Science has been pushed aside by statisticians anxious to prove their messages about health care systems.
Not only is health care and political correctness an oxymoron it is against our very much “cherished’ freedom of speech.
At this week’s National Prayer Breakfast Ben Carson M.D. gave a benevolent but strong message to the crowd,which included President Barak Obama and other leaders in government. about political correctness, and the serious danger to the United States of America.
Dr. Ben Carson teachs by example….and humor.
Thursday, February 7, 2013
Health Care Social Media Resource–Glossary
Thanks to Barbara Ficarra, R.N.,BSN, MPA Barbara Ficarra, RN, BSN, MPA, is an award-winning journalist, media broadcaster, speaker, medical blogger, consultant, media trainer, and health expert. She is creator, executive producer and host of Health in 30® Radio Show. Barbara is a registered nurse active on the front lines of health care: She is a head nurse at a level 2 trauma center and covers multiple medical and surgical units, critical care, oncology, cardiology and step-down units, the psychiatric in-patient unit and the Women’s and Children’s units, pediatric ER and Barbara has many years experience covering the main emergency room. Her clinical experience ranges from oncology to general medicine and surgery. Read more about Barbara. Barbara is a featuredwriter on Huffingtonpost.
20 Excellent Social Media Networking Resources for Health Professionals
- AMA Policy: Professionalism in the Use of Social Media
- Centers for Disease Control and Prevention (CDC) The Health Communicator’s Social Media Toolkit
- Cleveland Clinic Social Media Policy
- David Harlow, Esq. – HealthBlawg
- Deloitte – Social Networks in Health Care: Communication, collaboration and insights
- Healthworkscollective
- Healthin30/Social Media | Social Networking
- Found in Cache – Hospital Social Network List – Ed Bennett
- IBM Social Computing Guidelines
- Intel Social Media Guidelines
- Kaiser Permanente Social Media Policy
- KevinMD
- Lee Aase
- Mashable
- Mayo Clinic Center for Social Media
- New AMA Policy Helps Guide Physicians’ Use of Social Media
- Pew Internet & American Life Project, August 26, 2011
- Social Media Governance
- Social Media Today
- Web 2 0 Governance Policies and Best Practices
All of these websites offer guidelines for using socialmedia and setting a formal institutional policy
Wednesday, February 6, 2013
Unintended Consequence of the Affordable Care Act
The scenario: As written in the WSJ by David Lefffel M.D. (Yale University)
The Doctor's Office as Union Shop
Doctors have always been loath to strike, feeling a moral sensibility as to responsibility for their patients. And on a practical standpoint…the physician is the key producer in a medical business. Any type of work stoppage would be a self inflicted suicide gesture, for there is little wiggle room anymore in health financing.
Any strike would be self-limiting, short duration and largely a gesture as to physician discomfort with the evolving changes wrought by the Affordable Care Act.
As the country moves toward the effective start date of the Affordable Care Act in 2014, the operational and economic elements of this vast legislation are becoming clearer. Yet one likely outcome of the act that will directly affect the quality of patient care, and could affect its cost, has gone virtually unnoticed and unreported: the increasing trend for physicians to become employees, rather than self-employed. This development represents a potentially radical factor in the transformation of health care—the doctor as union worker.
Unlike hospitals, which operate under the rubric of large regulatory agencies, physicians have been much more difficult to regulate and monitor. For cost control to be effective, the professional autonomy and independent clinical judgment of the physician and other providers must in some measure be sacrificed to standardization. This can't be accomplished by overseeing thousands of doctors in thousands of offices and medical complexes, each conducting its own symphony.
The Obama administration, by intent or accident, has effectively driven a major change in the status of physicians. By reducing the reimbursement for certain office-based specialists while enhancing related payment to hospitals, the administration is compelling more and more physicians—many of them with an any-port-in-a-storm fatalism—to seek employment with health systems or large physician groups.
The change in the nature of physician employment will have effects never before experienced in America. As the effects of the Affordable Care Act come into focus, it becomes clear that when the majority of physicians are no longer self-employed—and barring any legislation to the contrary—their new employed status will provide doctors with the right to collective bargaining.
Leaders of the organized-labor movement already view service workers with nonexportable jobs as the last best hope of labor unions whose membership is at an all-time low. The truth is that physicians are now becoming service workers. They are well-educated and expensive to train, and their decisions have substantial significance in the lives of others. But doctors essentially provide a service, one that cannot be outsourced to India or China.
f doctors unionize, that raises an immediate question about their right to strike—the key lever in collective bargaining. That's a question for another day. For now, it's enough to contemplate what will occur when the practice of medicine becomes detached from its past as a profession—when doctors may in time come to see themselves not solely as healers but as workers, units of labor, in a system that is committed to delivering care to the greatest number.
When doctors occupy a service niche like the chambermaid in Las Vegas or the school teacher in Chicago, the expectations and compensation of the physician-worker will be defined in ways that may make the benefits of collective bargaining appear very attractive.
As has happened in other countries that have charted the course we are now on, a new reason for lack of access may at times be: "Office closed, doctors on strike."
Subscribe to receive immediate email notifications of Health Train Express Publication
Subscribe to Health Train Express by entering your email address in the box on the right banner. You will receive an email notification whenever it is published immediately.
Monday, February 4, 2013
Go Triple Aim !!
Accountable Care Organizations
I received my first copy of Accountable Care News for January 2013 Volume 4, No 1. Judging from the Volume number I have missed three years of activity among ACO proponents. Judging from my experience the vast majority of providers know little about ACOs.
Headlining the first page in the Banner is The Results of the Annual Accountable Care ePoll
According to ACN there are 150 ACOs participating in the Medicare Shared Savings Initiative serving more than 2.4 Million Medicare beneficiaries.
During early December 2012 Payers, Providers, MCOL and ACN sponsored a survey asking industry stakeholders their perspective on ACOs.
As in most new initiatives there are uncertainties as to how the new organizations will grow, and operate. The survey indicates some differences between 2011 and 2013. The survey which had a n=103 did not include anyone not already in an ACO, which highly biases the outcome.
In 2013 those who had the most optimistic outlook of ACO impact in the marketplace were vendors, with 56.7% saying that ACOs have or will have a significant market impact. 46 % of purchasers and providers felt the impact would be significant in the market place.
Will ACOs actually generate the necessary savings? Only 40% were confident while 31.8% were doubtful or very doubtful. Surprisingly providers had the greatest confidence levels 43.6%.
The “Triple Aim” a term bandied about now much like the DRG of the 1980s is a term coined by the Medical Advantage Group (MAG) to ascertain ACO readiness. Their criteria are developed from experience in developing one of the largest patient-centered provider network in Michigan. MAG
“Triple Aim “ was developed by the Institute for Healthcare Improvement (IHI and has become the framework for the NQ strategy of the U.S. Dept of HHS and the Centers for Medicare and Medicaid services
Triple Aim combines the pursuits of improving population health, improving patient experience of care, and reducing per capita costs.
1.Population health
2.Patient experience of care.
3. Reduction of per capita costs.
This term encompasses a vast collection of related and unrelated activities governed by the goal of 'Triple Aim”. Whether or not this term will be meaningful in the long run will be open to analysis as time goes on. Whether the criteria are called the Triple Aim or something else is moot. It seems more of a 'mantra' or cheer leading statement. For me it conj-ours up the spectacle of a thousand practice management experts at the next MGMA meeting chanting “triple aim.triple aim....triple aim and the next keynote speech of Donald Berwick (note: this writer does not intend to besmirch Dr. Berwick's stellar credentials and reputation as former head of CMS.
Let it be said however, that those following the 'enlightened path' should be cautious and analytical as the 'system'' becomes operative and adjust it accordingly. ACOs may very well fail to produce their intentions, however may be so thoroughly engrained in health systems that they will survive, with many 'workarounds' for it to operate at all. Defective organizations often survive in this manner, such as HHS, CMS and countless other inspired organizations.
There will be all sorts, sizes and shapes of ACOs…One model will not fill all. Some regions will be fertile ground for ACOs and in other regions ACOs will be inappropriate and fail to become established.
ACN goes on to say that there may be unintentional consequences in the market place. The growth of larger and larger provider organizations, stifling competition, and the acceleration of hospitals acquiring physician practices. Lawrence P. Casalino M.D.,PhD., M.P.H. elaborates his hopes for a pluralistic system with many choices for patients and providers.
Saturday, February 2, 2013
Accountable Care (Cost) Act
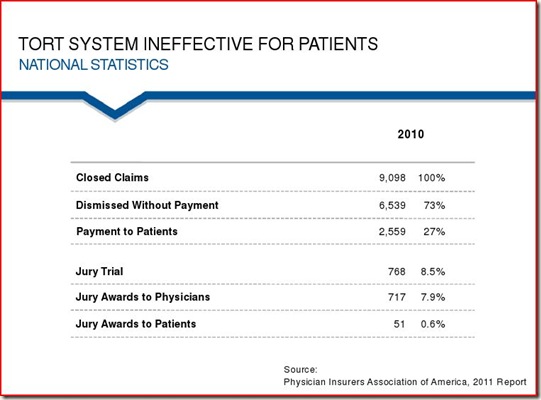
One of the biggest disappointments regarding Obamacare it its failure to address the impact of defensive medicine. The direct and indirect costs of medico-legal misadventures contributes to increased costs. Some are arguing that it is insignificant.
The Iceberg Effect
In an article written by Kathleen Baiker in Health Affairs she and her co-authors evaluated the Malpractice Liability Costs And The Practice Of Medicine In The Medicare Program (2007)
In addition to the observable financial figure, is the not so apparent and difficult to factor is the time/energy equation which diverts physicians from patient care where weeks and sometimes months are spent preparing defenses, attending depositions and court.
When one studies the exact nature and success rate of malpractice lawsuits, it becomes very apparent that the ‘injury'’ resulting in the lawsuit could be adjudicated in a better more professional and accurate way. It is often surprising to see just how often plaintiff’s do not gain financially as would be predicted. Juries often perform miscarriages of justice. Malpractice cases cannot be measured in terms of justice, right, wrong or terms of negligence.
A better model would be that of an investigative board, much like the National Transportation Board (NTSB) after an incident on public transportation. This investigative board would have the same subpoena and deposition power as a court of law.Fact gathering is performed by a variety of experts, presented to a board of review and a decision is rendered as to causation and assignment of responsibility for the event.
Tort Reform would reduce cost, and even more important it would increase the quality of care. Time and energy could be better spent evaluating diagnostic and treatment protocols.
The Medical Malpractice Tort system in the United States has three goals;
from; Presentation “Patients for Fair Compensation” given to Florida Medical Association by Richard Jackson and Jeffrey Segal M.D. J.D.
1. deterrence of unsafe practices
2. compensation for injured purposes and
3.corrective justice
The Tort System is not accomplishing these goals.
Sarah Z. Hoffman, ANNALS OF HEALTH LAW
The United States is unique in regard to medical malpractice.
Mold Problems...allergy, malaise
The number of people who are seeking treatment for Mold Toxin Illness (CIRS) is staggering. Given that 50% of homes/buildings in the US hav...

-
(click for locations) Or is it Doctor Google ? Either you are a lover or a hater of all things Google. Google however has some thing...
-
David’s Health Tech Newsletter: No. 62 – “Companies Disrupting Healthcare In 2015” via reddit.com The 21st Century has shown rapid develo...
-
At the intersection of health, health care, and policy.At the intersection of health, health care, and policy. A Four Years Into A C...